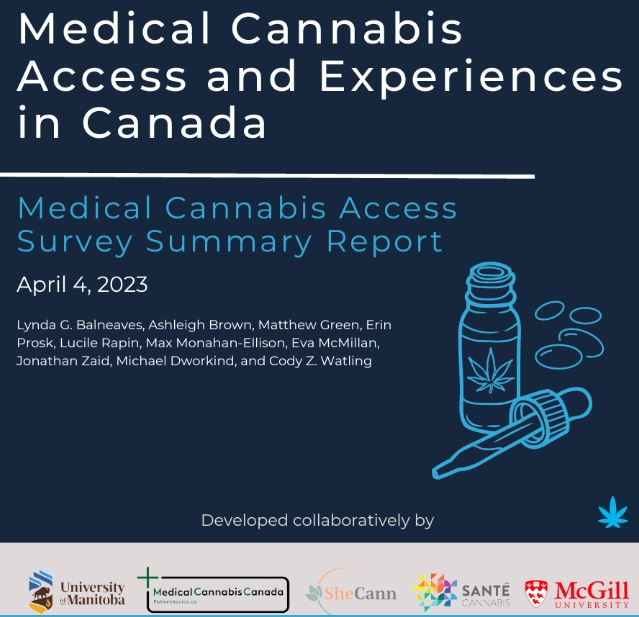
“Medical Cannabis Access Survey Summary Report” April 4th, 2023
Developed collaboratively by Lynda G. Balneaves, Ashleigh Brown, Matthew Green, Erin Prosk, Lucile Rapin, Max Monahan-Ellison, Eva McMillan, Jonathan Zaid, Michael Dworkind, and Cody Z. Watling
https://www.medicalcannabissurvey.ca/
Review By Jacqueline Kittel
Victoria Cannabis Buyers Club
Introduction
On April 4th 2023, we had the opportunity to listen in on a final presentation of the findings of the Medical Cannabis Access Survey conducted by independent third parties in Canada. The contributors included researchers from the University of Manitoba and McGill University, SheCann, Santé Cannabis, and Medical Cannabis Canada. This survey is not to be confused with the Health Canada survey we promoted in the fall 2022. The project we will be discussing today was conducted to capture, “the complex landscape of medical cannabis, access challenges and unmet needs among the patient community, supporting the importance of locating patients at the heart of consultations.” (pg 73).
This survey led by Dr. Lynda Balneaves of the University of Manitoba, seeks to distinguish between the experience of patients using cannabis with medical authorization (doctor approved) versus those without medical authorization. The survey points out the gaps in the current medical program, and how more resources can be allocated to find new and adaptive solutions to keep the medical program alive and well functioning. In this article we will look at how the Victoria Cannabis Buyers Club functions as a working model of a successful cannabis access point that meets all of the recommendations laid forth by these researchers.
Context
The Cannabis Act refers to the federal regulations that legalized recreational cannabis across Canada in October 2018. When the Act was implemented, a review process was built in and was set to take place 5 years post legalization. The time has come and an independent Expert Panel has been assigned by Health Canada to review the Cannabis Act as of September 22, 2022. The goal of the Expert Panel review is to assess the impacts of legalization, regulation, and access to cannabis for medical purposes among other metrics of success. This review is set to take 18 months and will complete in February 2024.
The independent survey we will be discussing today was conducted by researchers and patient advocacy groups; it is intended to be submitted to the Expert Panel as evidence of the current state of the medical cannabis program in Canada. The survey authors note that. “[t]he Cannabis Act is currently under review by a federally appointed Expert Panel, with no representation from patients, relevant clinicians, and researchers and minimal accessible opportunities for input on the medical cannabis framework.” (pg. 73) The survey data seeks to bridge the gap in patient representation by capturing the experiences of medical cannabis users and to argue for policy reform based on the findings to improve the medical cannabis program in Canada in the future.
At the VCBC we believe the information put forward from this independent study reflects what we already knew about the state of medical cannabis in Canada and reflects a reality that we deal with everyday. We have been in operation on the front lines since 1996, serving patients who are unable, or who can no longer, use legally authorized medical cannabis due to access and economic barriers. Our club continues to operate and push the boundaries because the legal available options are completely inadequate for the needs of medical patients in Canada.
The VCBC is a low barrier access point that has been successfully serving the needs of patients in our medical storefront and across Canada via the mail for 27 years. Currently the federal and the provincial governments are not taking seriously the value our medical model represents in providing access points and fighting the opioid epidemic. We will break down how we meet or exceed the recommendations of the survey authors below.
Survey Demographics (pg. 22)
- A total of 5,744 respondents completed the survey over the 5-month data collection period, of which 5,433 were currently taking medical cannabis.
- Of these individuals, nearly 62% of the sample identified as a woman, 33.1% identified as a male, and 3.9% identified as non-binary (1% missing data).
- The reported age of respondents ranged from 16 – 89 years, with an average age of 49.5 years.
- Most of the respondents reported their ethnicity as White (81.2%), with 5.9% identifying as Indigenous and 5.8% reporting mixed ethnicity.
- With regards to education, 92.8% of the sample reported achieving high school education or higher.
- Close to 30% of the sample reported a household income of less than $35,000 per year (before tax), which is below the low-income cut-offs for most households in Canada with a minimum of four residents
- Limitations: individuals who do not have ready access to the internet and/or have a device to complete the survey online were not able to participate in the study (e.g., homeless, living in poverty, incarcerated). The survey was also only offered in English and French (pg. 72)
The survey authors point out that of the respondents (n=5,433, 94.5%) who completed the survey, 54.1% reported having medical authorization (doctor approved use) whereas (n=2499, 45.9%) did not have medical authorization. This means that nearly half of the participants accessed their cannabis through Licensed Producers (LP) or other legal sources (designated growers, at home grow, legal recreational stores). Those with medical authorization also had a Health Care Practitioner (HCP) involved in their medical regimens with cannabis medicine. The other half of respondents did not have medical authorization, and did not have a HCP involved or were denied authorization by an HCP, and sourced their cannabis from legal recreational stores, community dispensaries, family and friends, online sources, or a dealer.
Barriers to Access
The medical cannabis program in Canada exists due to 30 years of activism from patients pushing the frontier by getting arrested and challenging cannabis charges via court decisions that forced government action. In 2018, Canada finally legalized recreational cannabis and in a lot of ways, medical cannabis has fallen to the wayside. This study acknowledges that there’s a drop off in registered medical cannabis users in Canada post legalization. Some factors for this decline include the convenience of in person retail recreational stores. A lot of users described that it was easiest to access their medicine at recreational stores but patients are simultaneously barred from asking any medical questions. The study found 51% of respondents received information about their medical cannabis and dosing via Google (pg. 51).
A lot of patients are unable to access medical cannabis or information due to HCP reluctance to authorize medical cannabis due to willful ignorance. It is not uncommon for a patient to speak to their doctor about medical cannabis and to get denied on benign grounds. “The reasons individuals reported their request being denied were centered on their healthcare professionals’ lack of knowledge about medical cannabis (50%), unwillingness to talk about medical cannabis (36%), and concerns about limited medical cannabis research (34%)” (pg. 10) This is not a just or equitable system to access cannabis if patients are subject to the whims and personal beliefs of doctor’s who are not required to learn about the therapeutic benefits of cannabis.
Very few respondents of the survey were able to get their medical cannabis covered by their insurance providers. “Across all current consumers of medical cannabis (N = 5,433), 55.7% of respondents reported having private health insurance (e.g., Canada Life Sunlife, Blue Cross) whereas 59.2% of those with medical cannabis authorization had private health insurance.” (pg. 51) What is alarming is that even though patients have a legally sourced and doctor authorized medical cannabis prescription, they are still getting denied insurance coverage.
The study found, “[o]f those individuals, only 170 participants, or 5.8% of individuals who held medical authorization reported being successful in the claims process” (pg. 50) That means that an abundance of patients who continue to use medical cannabis are choosing to pay out of pocket for this medicine due to its efficacy for their needs. Chronically disabled patients who live on excruciatingly limited budgets are still choosing to pay for this medicine. We collectively need to do everything in our power to lower or eliminate the costs for medical cannabis just like other prescription drugs in Canada.
The medical cannabis program is important but it needs to be made more effective for patients to use, starting with addressing the economic barriers. The study found 204 respondents stopped using medical cannabis because it was too expensive (pg. 36) Patients who access medical cannabis from Licensed Producers are required to order their medicine via the mail and pay for shipping. Medical cannabis is also subject to an excise tax, the same as recreational users. Therefore patients are simultaneously getting taxed extra for their medicine, they are buying it out of pocket with their limited budgets, and are being denied coverage from their health care plans.
The VCBC exists to bridge the gap between the barriers of the medical institution and patients’ needs for accessible and cost effective medicine. We are a non-profit medical compassion club and we provide low cost and low barrier medicine to patients in a store front, this is not currently allowed in the Cannabis Act. To sign up at the VCBC we need a proof of condition, it is a document that states what condition you are treating from a healthcare practitioner (GP, naturopath, chiro, nurse practitioner, etc). It does not require the patient to have a family doctor, which is a growing challenge for Canadians everyday, and it doesn’t require a patient to be fortunate enough to have a doctor that understands cannabis medicine.
The current medical colleges and universities still don’t teach medical students about the endocannabinoid system and the survey researchers pointed out that there is no centralized hub of cannabis information for doctors to learn. Therefore organizations like ours and other community dispensaries are present to offer education and product access to patients outside of the limits of the medical system until the system is improved holistically for patients everywhere.
Recommendations (pg. 74-76)
- DESIGN, IMPLEMENT, AND MAINTAIN A FORMALIZED EVALUATION OF THE MEDICAL CANNABIS FRAMEWORK IN CONSULTATION WITH PATIENTS AND KEY EXPERTS
- This data highlights the complex landscape of medical cannabis, access challenges and unmet needs among the patient community, but the Cannabis Act is currently under review by a federally appointed Expert Panel with no representation from patients, relevant clinicians, and researchers and minimal accessible opportunities for input on the medical cannabis framework.
- There is an unmet need for ongoing, sensitive, accessible, and specific consultation and information gathering with the diverse community of patients and caregivers, healthcare professionals, marginalized communities and other impacted groups on all regulations and matters related to the health, well-being and quality of life of individuals who take medical cannabis.
- This data highlights the complex landscape of medical cannabis, access challenges and unmet needs among the patient community, but the Cannabis Act is currently under review by a federally appointed Expert Panel with no representation from patients, relevant clinicians, and researchers and minimal accessible opportunities for input on the medical cannabis framework.
The VCBC has been a grass roots front line medical cannabis dispensary for the past 27 years. In that time we have built a wealth of knowledge when it comes to meeting patients where they are at, and providing medicine, services and education that makes their lives easier. We at the VCBC have invited the Expert Panel to come to our store in Victoria, BC to meet our staff and our community of patients. If the Expert Panel is serious about meeting the needs of patients, then we implore them to visit us because we are one of the very last medical compassion clubs still standing in Canada.
The voices of well off, predominantly white, and educated persons are most often heard when it comes to surveys and town halls. The voices of those without internet access, the voices of those facing opioid addiction, the voices of the elderly and the disabled were not amplified when cannabis was legalized in 2018. In fact, this survey even points out that it too isn’t able to even hear the voices of the most marginalized medical cannabis users (pg. 72) We want to showcase the perspectives of the patients whose lives are dependent on our continued work in the medical cannabis space. Small scale storefront medical compassion shops like ours are the answer to the gaps in the medical cannabis program to deliver in person tailored care and recommendations to patients in need.
- MAINTAIN REASONABLE ACCESS TO CANNABIS THROUGH A DEDICATED MEDICAL FRAMEWORK EMBEDDED WITHIN THE CANNABIS REGULATIONS
- This data highlights that Canadians using cannabis for medical purposes without medical authorization spoke to healthcare professionals less, relied more on internet and other non-evidence-based and unqualified sources of information, were less certain about how much medical cannabis they were taking, and were more likely to experience adverse effects and obtain medical cannabis from unregulated sources than individuals with medical authorization.
- The majority of respondents with medical authorization agreed that there was value in retaining the medical cannabis program as separate from the recreational cannabis market due to its unique exemptions, benefits, and products.
- This data highlights that Canadians using cannabis for medical purposes without medical authorization spoke to healthcare professionals less, relied more on internet and other non-evidence-based and unqualified sources of information, were less certain about how much medical cannabis they were taking, and were more likely to experience adverse effects and obtain medical cannabis from unregulated sources than individuals with medical authorization.
In November 2022, the Select Standing Committee on Health released a document titled, “Closing Gaps, Reducing Barriers: Expanding the response to the toxic drug and overdose crisis.” This document compiles the survey responses of healthcare providers and stakeholders across the country to assess how the government should approach managing the opiate crisis. In this review, the Standing Committee provides several recommendations on how to improve health care delivery to mitigate further opioid related harms.
“Several organizations, including the Public Health Association of BC, highlighted the need for low-barrier and culturally appropriate access to primary health care, which needs to include wraparound support. Resident Doctors of BC noted that clinical health care settings can be problematic, unwelcoming, or even triggering for some individuals who seek care for substance use, and added that anyone in the health care system can provide low-barrier compassionate care, not only physicians.” (Select Standing Committee on Health, pg. 58)
Medical compassion clubs with retail storefronts where members can access in person quality medical advice and information have been shut down and raided across this country since legalization. The federal government is denying patients access to culturally appropriate health care because our medical practitioners aren’t educated in cannabis medicine and recreational stores are not allowed to give medical advice. Medical compassion clubs like the VCBC provide services that legal operations are barred from providing due to the Cannabis Act regulations that aren’t in touch with the needs of patients.
Compassion clubs provide in person in depth health care orientations to welcome patients to cannabis medicine and to ask questions. They often do local delivery for those with mobility limits, provide access to high dose THC concentrated medicine for chronic pain, maintain smoking lounges for a safe consumption site, and offer a range of medical products to meet patients needs, including suppositories and topicals. Storefront medical clubs provide primary points of access for health care for patients who are new to cannabis, patients in need of guidance for chronic conditions, or those who are seeking alternatives to opioid substance use.
- IMPLEMENT CHANGES TO CANNABIS REGULATIONS, TAX POLICY, AND INSURANCE FORMULARIES TO REDUCE OUT-OF POCKET COSTS ASSOCIATED WITH MEDICAL CANNABIS AND RE-DIRECT USE AWAY FROM THE UNREGULATED MARKET
- Cost was identified as a substantial barrier to accessing cannabis for medical purposes. Canadians with the lowest income reported the highest out-of-pocket expenses related to medical cannabis. Medical cannabis is the only medication that is subject to excise duty and sales taxes. Participants who held medical authorization shared that removing sales tax would make it easier to access medical cannabis and reduce the use of unregulated sources. Individuals who had current medical authorization reported spending more on cannabis and only 5% indicated that they received some level of reimbursement for medical cannabis costs under any insurance plan or coverage.
- The tax burden faced by individuals should be addressed through the elimination of sales taxes and reforms to federal excise duty directed towards benefitting those who take medical cannabis. Private and public payers are encouraged to review the status of medical cannabis on their formularies and consider expanding covered indications. Employers should also consider adding medical cannabis as part of their group benefit plans.
- Cost was identified as a substantial barrier to accessing cannabis for medical purposes. Canadians with the lowest income reported the highest out-of-pocket expenses related to medical cannabis. Medical cannabis is the only medication that is subject to excise duty and sales taxes. Participants who held medical authorization shared that removing sales tax would make it easier to access medical cannabis and reduce the use of unregulated sources. Individuals who had current medical authorization reported spending more on cannabis and only 5% indicated that they received some level of reimbursement for medical cannabis costs under any insurance plan or coverage.
By refusing to issue cannabis a Drug Identification Number (D.I.N.), the government has created a situation where cannabis is authorized for use by doctors but not actually prescribed. Without a D.I.N., doctors can state that there has not been enough research to prove that cannabis is safe to use as medicine, giving Health Canada justification to add the excise tax to medical cannabis.
This same sin tax is applied equally to medical cannabis as it is recreational cannabis. It is immoral and wrong to charge a sin tax on medicine that is prescribed to patients from their health care practitioners. If Health Canada is concerned with getting cannabis out of the hands of the black market, then charging an excise tax is an extremely efficient way to prevent consumers from buying in the legal market. The attempt to bolster a legal cannabis industry is completely undermined by an unnecessarily high tax rate on this consumer good.
At the VCBC we pay GST tax on our products that are sold in the store. We also contribute large sums of our cash flow to payroll deductions and contributions to EI and income tax because we pay a living wage for the staff that run the shop every day. When the VCBC was raided for the third time by the CSU on March 23, 2023, it was the Victoria Police Department that took the cash money from our safes. They took approximately $32K from our store, of which approximately $19K was earmarked for our monthly GST and payroll deductions.
Lastly, the prices being charged for most edible products by LPs is completely disproportionate to the cost of production and are entirely based on generating maximum profit. For example, the VCBC sells its 75 mg THC cookies for $2.50, a stark comparison to the common price of $12 to $14 per 10 mg cookie that legal stores offer. Clearly the cost of the THC and the cookie are a fraction of the prices being charged but these firms have built their revenue projections for shareholders upon these exceptionally high prices and unrealistic sales numbers, collectively setting the profit margins on edible products dramatically higher than other items. Medical cannabis should not be profit driven and should be provided due to the humanitarian need for a low impact medicine with few downsides for countless patients.
- DEVELOP, IMPLEMENT, AND EVALUATE HEALTHCARE PROFESSIONAL EDUCATION TRAINING FOCUSED ON MEDICAL CANNABIS ACROSS THE MULTIDISCIPLINARY HEALTHCARE TEAM
- Respondents perceived a lack of knowledge among healthcare professionals about cannabis for medical purposes.
- The majority of individuals who were denied a medical authorization to take medical cannabis perceived a lack of understanding or stigma from their healthcare professional as key reasons. The recent survey of healthcare professionals by Health Canada found around half of clinicians are not well informed about the usage of cannabis for medical purposes and do not recommend cannabis as a therapeutic option due to lack of information about dosage (19).
- With funding support and resources from federal and provincial/territorial government agencies, healthcare professional regulatory colleges and training programs are encouraged to collaborate on the development of key competencies needed to provide safe and informed care related to medical cannabis.
- Inclusion of medical cannabis on healthcare professional credentialing exams, and the creation of medical cannabis curricula for the diverse healthcare professional community in Canada is needed.
- Respondents perceived a lack of knowledge among healthcare professionals about cannabis for medical purposes.
We at the VCBC completely agree with the recommendation to develop, implement and evaluate health care professional training programs focused on medical cannabis. It must be pointed out that cannabis was under prohibition for a century. In that whole time research was denied and stigma flourished to demonize this plant. The effects of that stigmatization are deep and our government is doing next to nothing to address it on a systemic level or to take cannabis seriously as a medicine.
As we described above, cannabis does not have a D.I.N. number and therefore cannot be prescribed. Additionally, medical students are not required to learn anything about the endocannabinoid system and are not tested on cannabis at all in their final exams and we are decades into medical cannabis being legal in Canada.
Public education on cannabis continues to focus on mitigating the potential for harms from low dose cannabis use. Instead of focusing on cannabis’s revolutionary potential to replace alcohol or other drug use, cannabis continues to be portrayed as a risky substance. Emphasizing the potential harms of cannabis while ignoring or diminishing the potential benefits has stopped many from using cannabis, or dosing themselves properly. The fear based messaging from Health Canada has stopped many from trying this effective treatment for their stress, anxiety, pain or other ailments.
Ultimately, the lack of re-education of our health care practitioners is a major underlying failure of Health Canada in their public education efforts. Physicians continue to deny patients prescriptions for cannabis or to authorize patients’ use of medical cannabis. HPC’s lack of understanding, often willful ignorance, of cannabinoids or terpenes means that when a patient or a general consumer has a question about cannabis, they can’t get reliable information from a recreational store or their doctor.
For the 470 individuals who tried to get authorization in the past but were not successful, the reasons they reported for their request being denied included their healthcare professionals’ lack knowledge about medical cannabis (50.1%), their refusal to talk to them about medical cannabis (35.8%), their concerns about the lack of research related to medical cannabis (33.7%), and their suggestion to try different treatments (25.5%). Other reasons these respondents did not seek medical authorization included the perception that there was no need due to the existence of the recreational cannabis market (48.9%), the fact that they couldn’t find a healthcare professional to speak to about medical cannabis (45.1%) and being unsure how the medical cannabis program worked (40.6%) (pg. 38)
To effectively educate the public on cannabis and its uses, Health Canada should look to improve how it educates its doctors. By increasing the education, and requiring the colleges to teach about the endocannabinoid system, more people will learn how to use this medicine effectively from informed health care providers. Empowering citizens through informed health care is more effective than relying on public ad campaigns as the ultimate tool to educate the masses.
- EXPAND REASONABLE ACCESS TO MEDICAL CANNABIS BY ADDING COMMUNITY PHARMACY DISPENSING
- Currently, there are no or very limited dedicated in-person access points for medical cannabis designated under the Cannabis Regulations. Respondents highlighted the lack of in-person access points for medical cannabis as a challenge and identified a need for community pharmacy dispensing of medical cannabis and evidence-based information.
- The majority of respondents reported taking medical cannabis alongside other medications. There are possible drug-drug interactions and safety considerations that must be considered when using medications, including cannabis, which require oversight from pharmacists.
- The expansion of medical cannabis access through community pharmacies would encourage consultation with pharmacists about the efficacy, safety, and appropriate product usage of medical cannabis, as well as address delays in receiving cannabis products.
- Currently, there are no or very limited dedicated in-person access points for medical cannabis designated under the Cannabis Regulations. Respondents highlighted the lack of in-person access points for medical cannabis as a challenge and identified a need for community pharmacy dispensing of medical cannabis and evidence-based information.
Medical storefronts for cannabis are not allowed under the Cannabis Act. If a patient wants to access medical cannabis they first have to have a doctor, which is a big challenge for Canadians today. Then that doctor has to believe in cannabis. Then the patients must have exhausted all other treatment options and the side effects, before the doctor can consider medical cannabis.
If a patient is lucky enough to have a doctor, and to have a doctor that understands and values cannabis medicine, they are then able to be authorized for medical cannabis. Then the patient has to have a credit card and internet access to order low dose and high cost medicine online. The medicine then has to be shipped to a home address, not including a PO box. How many obstacles does a patient have to go through?
Prior to legalization in 2018, patients had the privilege of an abundance of local small scale dispensaries and compassion clubs to access cannabis in their neighborhoods. Patients were able to build relationships with their budtenders and they could ask for advice and recommendations from an informed individual who could provide tailored care and comprehensive answers. This model is not allowed in the current medical framework and unlike the researchers, we disagree that community pharmacies are the answer.
In the opioid harm reduction community there is a tendency to want to include HCPs and nurses and pharmacies into the dispensing of safer supply of medicines. However, the desire to rely on this existing medical institution only provides the appearance of safety and comfort. The reality is that the medical establishment is slow, mired with bureaucratic red tape, and it is still inaccessible to patients and those on the fringes.
There are many reasons why medical storefronts provide a much better resource for patients than recreational stores. Compassion clubs like the VCBC focus on products designed for medical uses, educate staff about the various applications of their medicines and provide patients with a friendly space to ask questions without feeling rushed or pushed towards a sale for profit. Clubs can also open a consumption space, offering patients a relaxing opportunity to use their medicine, meet other people suffering from similar medical problems and learn more about the products available in the facility.
Staff working in medical dispensaries are often patients themselves, giving them personal experience with using the products for various medical ailments Since these staff have medical needs they often are the first to try new products, try various vaporizing devices and learn about how others are benefiting from cannabis use in their personal and professional life. This connection between patients and other patient/caregivers builds a strong bond of trust and companionship that generates a feeling of togetherness that does not normally happen in retail or health care facilities.
A program educating budtenders on the various medical applications of cannabis would be necessary to have national standards for dispensing cannabis as medicine based on existing research. This accreditation system would help ensure a broad understanding of the products available to patients is made known to those dispensing it at storefronts across the country. Patients would greatly benefit from having direct conversations with experts in local facilities and medical retailers would need a clear method to ensure staff are educated in the basics of cannabis medicines.
Patients deserve the best medical cannabis program possible, not one that borders on meeting constitutional standards. Licensing compassion clubs like the VCBC would drastically improve the medical cannabis program, providing better healthcare without negatively affecting public safety. Over all of these years of excluding compassion clubs from its programs, Health Canada has never provided a reason for this obvious gap.
- MAINTAIN AND AMPLIFY A FEDERAL RESOURCE HUB THAT PROVIDES UPDATED, EVIDENCE-BASED INFORMATION AND RESOURCES ABOUT MEDICAL CANNABIS
- In this study, the majority of respondents reported using Google to find information on cannabis for medical purposes. A substantial proportion also reported being unaware about the medical cannabis program in Canada.
- Existing healthcare professional resources developed by Health Canada have not been updated since October 2018 (3). As clinical evidence on medical cannabis continues to increase, resources need to be updated on a regular basis for healthcare professionals and institutions.
- Effort should be made to develop a federal resource hub that is accessible to all Canadians, contains updated and evidence-based information, forms, and algorithms that are informed by clinicians and researchers, and individuals with lived experience of taking medical cannabis.
- To support the development of evidence to inform clinical decision making about medical cannabis, a well-funded, coordinated national research strategy focused solely on medical cannabis is urgently needed.
- In this study, the majority of respondents reported using Google to find information on cannabis for medical purposes. A substantial proportion also reported being unaware about the medical cannabis program in Canada.
There is a lot to know about medical cannabis, it is unlike a lot of other medicines and every person needs a slightly different dose, strain or method of consumption. When it comes to oils, there’s a lot of difference between a crude full spectrum oil and a highly refined isolated oil. There is a lot of information about dosing, titrating medicine for cancer users, and using different medicines for different conditions on different days. Therefore we agree with the recommendation to create a centralized source of up to date information for all stakeholders.